Dental X-ray practices
The purpose of this guideline is to facilitate the interpretation of radiation legislation and, thereby, to promote radiation safety in practice. This guideline is not binding as such, but they reflect STUK's view on how the requirements of radiation legislation can typically be met in different circumstances. The requirements of the legislation can also be fulfilled otherwise. Operators must consider how the instructions apply to their own practices on a case-by-case basis. Guidance is also given on practical measures and means to reduce the radiation exposure caused by the practice, where possible.
A special feature of dental X-ray examinations is that often the dentist treating the patient determines the need for the examination and also performs the examination or at least is responsible for the imaging practices and the radiation exposure caused to the patient. The justification for X-ray examinations must always be considered patient-specifically. While in dental X-ray practice the referrer is often the same as the person performing the imaging, it is especially important that this person is familiar with good international and national practices and follows radiation-safe working methods. The self-assessment of operations and the monitoring of the development of dental X-ray imaging as well as new information and the principle of continuous improvement are also emphasized.
Dental X-rays are typically taken in dental treatment rooms, which are already designed at the beginning of the operation so that there is practically no radiation outside the room.
Those performing the examination must protect themselves so that they are not unnecessarily exposed to radiation. When imaging with an intraoral X-ray equipment, the operator usually does not need additional protective equipment as long as they avoid the area of the primary beam during the examination and stay at least two meters away from the patient and the X-ray tube. However, it is recommended to move behind a wall that shields from radiation during the examination. In panoramic imaging, it is advisable to move behind the wall and use a mirror or lead-glass window to monitor the patient. In this way, the operator can avoid additional radiation exposure.
If a person needs to be in the imaging room close to the patient, it is recommended that they use separate radiation shields, such as a movable radiation shield or a lead apron. The dose caused by cone beam computed tomography (CBCT) equipment may be similar to that caused by panoramic examinations or, depending on the examinations, it may be several times higher. For this reason, imaging should always be performed from behind a radiation shielding wall or from a separate control room so that the operator has visual contact with the patient either directly or through a mirror.
Radiation protection of the patient
Dental X-ray practices are well established, and the doses caused to patients by intraoral X-ray devices and panoramic imaging equipment are low, so the risks caused by radiation can be kept very low. Limiting the radiation field is the most significant way to reduce the exposure of the patient. For intraoral imaging, the radiation dose received by the patient can be reduced by using a rectangular radiation beam the size of the radiation detector. In panoramic tomography, cephalostat and CBCT examinations, it is also important to limit the radiation beam according to the area of interest and patient size. The imaging parameters used should also be optimized for the subject. Modern equipment have automatic dose adjustment capabilities that help the user optimize the imaging.
Patient contact shielding, such as a collar-shaped thyroid shielding, is not necessary for dental X-ray examinations, as the shielding does not significantly reduce the patient's radiation exposure. Shielding may also interfere with the examination or result in a need to repeat the imaging.
The radiation exposure to the fetus during dental X-ray examinations is very low and, when considering the need for dental imaging, there is no special need to take into account the patient's possible pregnancy. A lead apron placed on the abdomen therefore does not have a significant shielding effect, and using one is not necessary.
Performing the examination
Where radiation is used, there has to be written instructions for carrying out normal X-ray examinations. The instructions must be sufficiently detailed to enable the operator to perform the examination successfully and safely.
In dental X-ray practice, examinations are often also performed by healthcare professionals that are trained for X-ray examinations, but they are not a dentist or a radiographer. Adequate information on radiation protection must be available for carrying out the examination, but also sufficient user training with the equipment in use. The operator must ensure the necessary induction and supplementary training of the personnel.
Use of the Radiation Safety Officer, Radiation Safety Expert and Medical Physics Expert
In dental X-ray practice, the Radiation Safety Officer may be a dentist, radiographer, medical doctor or medical physicist. The radiographer and doctor must have completed the separate training that qualifies for Radiation Safety Officer in the applicable field of expertise.
In the medical use of radiation, a medical physicist can act as a Medical Physics Expert or a Radiation Safety Expert. In dental X-ray practice, the medical physicist can, if necessary, provide advice on matters related to the radiation protection of patients, workers and the general public as well as on the design of the place of use. If only intraoral X-ray equipment, cephalostat or panoramic tomography equipment is used, continuous use of a medicall physicist is not required. However, if there are known changes in operations, for example, with regard to the places of use or radiation exposure, or if there are plans to introduce portable X-ray equipment, it may be necessary to consult an expert.
In the case of CBCT equipment, there is a greater need for a madical physicist at the beginning and during the operation, for example, in the optimization and determination of patient doses.
Radiation safety deviations
In dental X-ray practices, the additional exposure caused by a single radiation safety deviation is rather small. However, possible radiation safety deviations and measures to prevent them should be considered in advance from the point of view of one's own operations. A radiation safety deviation may be, for example, a malfunction of a device that prevents the image formation due to a connection error and, therefore, causes additional exposure to the patient. Imaging of the wrong patient and the exposure of personnel or an external person are also considered radiation safety deviations. On the other hand, even if the repeated imaging causing additional exposure is required due to the patient's movement, it is not classified as a radiation safety deviation but as part of normal operations. It is important to deal with the deviations that have occurred internally and to find out their causes and how to prevent similar deviations in the future.
Typically, radiation safety deviations from dental X-ray practices do not need to be reported immediately, but they can be reported to the Radiation and Nuclear Safety Authority (STUK) as annual notifications. For example, a radiation safety deviation that must be reported to STUK without delay is a theft or loss of a radiation appliance or a technical failure of the equipment that systematically causes additional exposure.
In dental X-ray practice, quality assurance refers to all the measures taken to ensure that a defined, necessary and sufficient level of quality is achieved. The operator sets its quality objectives and defines, for example, the targets for self-assessment. The quality assurance programme must include the quality assurance measures, the intervals and responsibilities concerning their performance, the action levels and the measures to be taken when the levels are exceeded. Quality control is carried out at predetermined intervals, after significant repairs or maintenance and whenever there is reason to suspect that the operation of the equipment has been disturbed or changed. The results of the quality assurance measures must be documented. Guidance on the various aspects of quality assurance can be found in the following sections.
In intraoral imaging, quality assurance includes the annual self-assessment of activities, which must be carried out in all medical uses of radiation. Topics for self-assessment include, for example, the implementation of the guidelines and practices concerning the performing of the examination and treatment according to the plan or the systematic assessment of clinical image quality. Although the assessment of the clinical image quality of intraoral equipment is not required in the legislation, it is nevertheless a good target for self-assessment.
In panoramic and CBCT imaging, in addition to self-assessment, patient dose determination (at least every three years) must be performed and the dose display of the device can be used to determine it. The reliability of the dose display must be verified at regular intervals, for example, in connection with scheduled maintenance. The average patient dose determined at the place of use for a specific examination must be compared to the reference level for that examination. The reference level refers to a predetermined dose level that is not presumed to be exceeded in an examination performed according to the standards of good practice upon a patient of normal size. STUK provides reference levels for the most common examinations through separate decisions, and these will be updated as necessary. If the average patient dose in the examination exceeds the reference level, the reason for this must be investigated and the dose must be reduced if it is possible from the point of view of sufficient image quality.
The clinical image quality assessment must be performed every two years for panoramic and CBCT imaging practices. Clinical image quality assessment refers to the regular assessment of patient images, in which, for example, patient images taken over a certain period of time are reviewed, documented and compared with generally accepted good image criteria. In addition to a separate clinical assessment of image quality, the quality of the images taken of patients is continuously monitored visually immediately after the examination. However, observations made in daily work are not routinely recorded and, on the other hand, the evaluation criteria for them are not predetermined. These individual image reviews are not comparable and therefore do not meet the objective of quality control of clinical patient images.
In CBCT imaging, clinical audits may also be required if the classification of medical exposure specified in the safety assessment is 2. The aim of both the self-assessment and the clinical audit is to ensure that the unit complies with radiation-safe working methods and produces images with diagnostically high enough quality. In a clinical audit, the X-ray practices are reviewed from the preparation of referrals all the way to the patient's treatment. An internal clinical audit complements the self-assessment of the operations and is carried out every four years in activities where the classification of medical exposure is 2. An external clinical audit is carried out every eight years in activities where the classification of medical exposure is 2. External clinical audits are carried out by a group of qualified and experienced experts independent of the operator.
Acceptance inspection and commissioning of x-ray equipment
The instructions and other documents related to the use of the equipment must be provided with the equipment. For example, the user manual, technical manual, installation manual and other possible documents are integral parts of the equipment. If there are shortcomings in the instructions and documents of the equipment, the delivered equipment can be considered to be incomplete. The manuals must also correspond to the supplied hardware and software versions.
X-ray equipment must undergo an acceptance inspection before it is actually put into operation. The operator is responsible for ensuring that the acceptance inspection has been carried out, but usually the inspection is carried out by the supplier of the equipment. The acceptance inspection ensures, among other things, that the equipment functions appropriately and safely after the transport and installation so that the statutory requirements and the key performance and safety characteristics stated by the manufacturer are met. Issues being inspected include, for example, the accuracy of the radiation beam with alignment light, the accuracy of dose display as well as inspections of the radiation output characteristics, such as the accuracy, repeatability and linearity of the tube voltage (kV), tube current (mA) and imaging time (s). During the acceptance inspection, the reference performance values for the performance of the equipment are also determined.
The supplier often organizes user training, the scope and timing of which should be determined already when purchasing the equipment. In the training, special attention must be paid to the new features of the equipment and the features that have changed compared to any previous equipment, such as general equipment safety and the ratio of the imaging parameters used to the sensitivity of the imaging detector.
Checking the mechanical functioning of x-ray equipment
The mechanical functioning and condition of the x-ray equipment should be monitored continuously when using the equipment. For example, the persistence and centering of the orientation or positioning of the x-ray tube and the condition of the cables of the equipment should be monitored in normal imaging situations. The operation of any emergency switches and warning lights must be checked by testing.
Ensuring the operating condition of the X-ray equipment
Verification of the technical performance of the X-ray equipment must be carried out periodically. This ensures the operability of the radiation equipment and the sufficiency of the performance characteristics throughout the service life of the device. Ensuring the functionality of the equipment requires special technical expertise and special equipment, such as radiation meters and quality control phantoms. Therefore, the verification is usually done by the equipment supplier's maintenance service or other maintenance service. Intraoral X-ray devices do not have a defined frequency for performance testing. Tests to verify the operating condition must also be carried out if there are any doubts about the equipment's performance on the basis of a test carried out by the user. The in-use acceptability requirements concerning panoramic X-ray equipment and CBCT equipment must be verified every 24 months.
Tests by users
User tests are easy, relatively frequently used tests that are usually performed by the personnel using the equipment. User tests are divided into safety tests and functional tests. Safety tests include checking the mechanical functions and emergency switches of the X-ray equipment, the operation of radiation detectors and warning lights and checking the condition of radiation shields. Functional tests include the imaging of the test piece and image analysis, checking the alignment, size and homogeneity of the beam and the aiming of the light signals.
To assess the quality of the image, an X-ray (test image) of a suitable test piece (phantom) is taken in the same manner, always using the typical imaging technique used in clinical imaging and the same imaging values. The test piece should be such that, on the basis of the image taken of it, the uniformity and quality of the image produced can be assessed. The test image is compared visually with a reference image previously taken with the same imaging technique and values. In the comparison, attention can be paid to image uniformity, contrast and resolution as well as possible image errors.
A test image taken with panoramic tomography or CBCT equipment can be used to check, in addition to the image quality and the size of the radiation beam, the smoothness of the movement of the X-ray tube and the image detector. In addition, it can be used to ensure that the patient can be positioned correctly for the imaging, i.e. to check the orientation of the patient's positioning lights. The test is carried out in accordance with the manufacturer's instructions.
The test image with the image quality phantom must be taken with intraoral X-ray equipment every 12 months and with panoramic tomography and CBCT equipment every 6 months. Equipment-specific phantoms are usually delivered together with the equipment or can be ordered separately from the manufacturer's representative/maintenance.
Quality control of imaging receptors
It is important to monitor the proper condition of image receptors and image viewing devices and equipment in order to ensure sufficient image quality. The best instructions for performing adequate quality control can be obtained from the equipment manufacturer. For example, for flat panel detectors, equipment manufacturers recommend periodic uniformity calibration to ensure the uniformity of the image.
Digital imaging plates should be protected against scattered radiation. Imaging plates that have been exposed to radiation or have not been used for a long time should be emptied before they are used for imaging. Imaging plates should be read within a reasonable period of time after the examination in order to avoid image fading and poor image quality caused by the accumulation of additional background radiation. The cleanliness and condition of the imaging plates must be inspected visually. If necessary, the imaging plates are cleaned in accordance with the manufacturer's instructions.
Recommendation on image viewing environment and image monitor quality control
The operation of the monitors should be assessed with the help of possible test images and programs on the image viewing workstation. Test images can be used to check that the monitor meets the specifications promised by the device manufacturer. By comparing the results of the assessment with the previous results, it is possible to see if the monitor features have changed and impaired its performance.
The viewing conditions of the image are linked to the lighting of the room, and it is important to pay attention to the reflections visible on the screen of the monitor. The viewing conditions can be checked by paying attention to the position of the monitor and the viewing angle. For example, the monitor must not show reflections of light sources when viewing a dark or black screen. The room should also be dim enough for viewing x-rays so that contrast differences in dark areas can be observed.
For the purpose of a weekly inspection by the users, it is often sufficient to establish that no changes have taken place in the lighting or arrangements of the room. The monitor should not be exposed to direct light from other light sources, such as lamps or windows. In addition, these light sources should not be in the visual field of the image viewer.
The quality assurance concerning the primary monitor, i.e. the image viewing monitor, which enables the doctor to give a statement or which is used to make a treatment decision, must be carried out once a month, for example, using a suitable test image.
Inspecting the condition of protective radiation shields
When radiation shields are stored in places reserved for them, for example, in racks intended for radiation shields, the shields will retain their shape and their maximum service life. The condition of radiation shields can be verified first by checking any damage manually and visually. This ensures that the protective material has remained in place. It is also checked whether the cover fabric and seams of the radiation shields are intact.
When an individual radiation safety deviation occurs in intraoral X-ray operations, the additional exposure caused by it is relatively small. In practice, only in exceptional cases may it be necessary to determine the radiation exposure more precisely than based on a literature assessment.
Preparation
The operator must identify in advance what types of radiation safety deviations may occur. On this basis, the operator must take adequate measures to prevent deviations. For example, the classifications presented below can be used as summary information on radiation safety deviations to be reported to STUK without delay. Identifying and preventing radiation safety deviations is part of the safety assessment.
The operator must also include a plan for the following in the quality system, for example in the safety assessment of radiation activities:
- How are radiation safety deviations handled and recorded?
- What is the estimate of the radiation exposure caused based on?
- Who will report a radiation safety deviation and to whom?
- When and how can you get advice from a hospital physicist if a patient, staff member or external person is exposed to a significant degree?
Handling a radiation safety deviation
In the event of a radiation safety deviation, it is important that those involved in radiation activities process the event and find out the reasons behind it. The operator should also examine how similar deviations can be prevented in the future.
Typically, individual radiation safety deviations in intraoral x-ray operations are reported to STUK annually as summary data. Summary information on intraoral x-rays is provided on the following events and underlying factors:
- wrong patient imaged because the referral was made to the wrong person
- human error
- other reason
- error in the imaging because of an error in the referral data
- human error
- other reason
- wrong person imaged
- the patient’s identity was not verified before the imaging
- other reason
- wrong imaging done
- human error
- imaging failed (for non-patient related reasons)
- incorrect or incomplete instructions
- human error
- hardware or operating error
- other reason
- unnecessarily repeated imaging
- no prior knowledge of previous examination
- other reason
- worker unnecessarily exposed to radiation
- an external person (i.e. a representative of the population) has been unnecessarily exposed to radiation
- other radiation safety deviation or near-miss
In addition, for each type of radiation safety deviation, the operator must briefly record the measures taken to prevent similar events in the future.
The annual report can be submitted using the form on the STUK website (link to form will be added later).
Certain radiation safety deviations in intraoral X-ray operations must be reported to STUK in writing without delay, at the latest within two weeks of the occurrence. A report must be filed without delay if at least 10 patients are subjected to systematic deviating exposure in CBCT imaging and the average magnitude of this exposure deviates from the planned exposure by at least 50%, or the additional effective dose caused by the event is at least 1 mSv.
A report must also be made without delay if the X-ray unit is lost, stolen, used or held without a safety licence issued by the Radiation and Nuclear Safety Authority.
Radiation and Nuclear Safety Authority (STUK) supervises dental X-ray practices through monitoring survey. In 2025, STUK sent a monitoring survey about dental X-ray use to 265 safety licence holders. The aim of the survey was to share information on the requirements and best practices of radiation use. With the help of the guiding text in the monitoring survey, STUK sought to illustrate radiation safety requirements as concretely as possible. The purpose of the survey was to survey the implementation of radiation safety while ensuring that safety licences are up to date.
Target groups of the monitoring survey
In 2025, STUK sent monitoring surveys to both private and public sector licence holders. The monitoring survey primarily focused on safety licences that had not undergone inspections by STUK in recent years. The size of the licence holders ranged from one-dentist clinics to large organisations.
All of the recipients of the survey had intraoral imaging services in their safety licence. In addition to intraoral imaging, 135 of the licences included panoramic X-ray units. A further 5 licences included CBCT examinations.
Monitoring survey findings
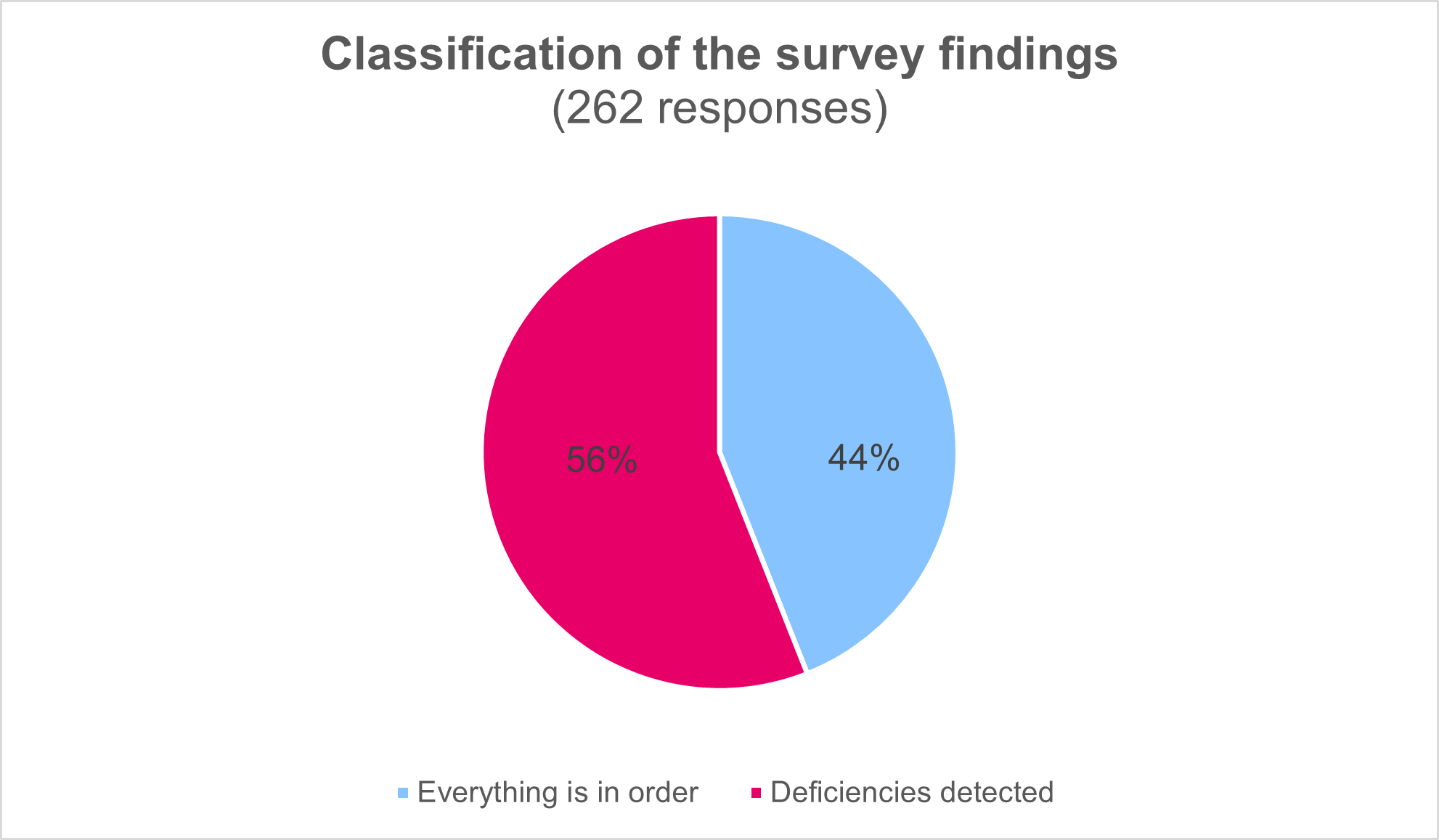
In 2025, the survey was answered by 262 respondents (response rate 98,9%), of who three reported that their radiation activities had ended or were currently on hold. Three license holders did not respond to the survey. The monitoring survey examined topics related to the management system of a radiation practice, safety assessment concerning a radiation practice, radiation safety deviations, quality assurance of radiation activities and supplementary training. As a rule, the situation is well in order, as a large majority answered all the questions in the survey by stating that the matter in question is in order. In summary, the majority of the respondents have taken the key requirements of radiation safety into account and are committed to acting accordingly.
Up-to-datedness of licence information
However, the survey revealed that dental X-ray licence holders have deficiencies in, for example, the up-to-datedness of safety licence data, documentation and quality assurance. One of the most important findings was that some licence holders did not have up-to-date information on safety licences. 12% of the respondents reported that the information in their safety licence was not fully accurate, especially the information regarding the radiation safety officer (RSO) was outdated. It was also found that amendments to licences, such as X-ray equipment removals and changes in location data, had not always been reported to STUK.
Up-to-datedness of radiation-related documents
According to the respondents, the requirements related to supplementary training were not always met, and deficiencies were particularly noted in the record-keeping of supplementary training. According to the 2025 survey, approximately 16% of respondents did not maintain individual records of employee-specific supplementary training for personnel participating in radiation activities.
The documents related to the management system and safety assessment of radiation practices are up to date for the majority of respondents. However, there are deficiencies in the content of the documents; for example, approximately 27% of respondents reported that the arrangements for using the Radiation Safety Expert and the Medical Physics Expert (MPE) were not described in their management system.
Deficiencies in quality assurance
The responses to the survey also revealed deficiencies in quality assurance programmes. Based on the responses, there were deficiencies in different areas of quality assurance, but the most common shortcomings concerned in particular technical quality assurance and monitor quality control. In 2025, approximately one quarter of respondents reported that they had not performed quality control of monitors in accordance with the requirements. Many missed an annual luminance check, in particular, which requires special equipment and maintenance services. Image quality screening and equipment maintenance arrangements were also inadequate for some operators.
According to the responses, 3% of the respondents do not carry out a self-assessment annually, even though it is an important part of self-monitoring. As underlying reasons, organisations may have insufficient resources to develop their operations. If no systematic self-assessment is carried out, safety-related deficiencies may not be detected in time.
STUK measures due to the monitoring survey findings
Most of the responses to the 2025 monitoring survey (56%) were processed by STUK by sending an individual feedback message to each respondent, depending on what kind of findings STUK made on the responses of the licence holder in question. In the feedback, the licence holders were also given instructions on how the observed deficiencies should be rectified to meet the requirements of radiation legislation. Those licence holders who had all the survey topics in order (44%) based on the responses received an email acknowledgement from STUK for responding to the survey.
In 2025, STUK did not identify any serious deficiencies in the responses to the supervision survey that would have required STUK to issue a binding decision to rectify the licence holder’s shortcomings.